How to Choose Between Generic Medications When Multiple Options Are Available

Not all generic drugs are the same - here’s how to pick the right one
You’ve been prescribed a generic medication, and when you pick it up at the pharmacy, you’re handed three different bottles - all with the same active ingredient, same dose, same shape, but different names on the label. One costs $5, another $8, and the third $12. You’re confused. Aren’t generics supposed to be identical? Why does it matter which one you take?
The short answer: they’re mostly the same, but not always. And for some people, the difference matters more than you think.
Generic drugs are required by the U.S. Food and Drug Administration (FDA) to contain the same active ingredient, strength, dosage form, and route of administration as the brand-name version. They’re also required to be bioequivalent - meaning they deliver the drug into your bloodstream at nearly the same rate and amount. That’s the rule. But here’s what no one tells you: bioequivalence doesn’t mean perfect identity. It means within a range.
What bioequivalence really means (and why it’s not as simple as it sounds)
The FDA says a generic must deliver the active ingredient into your blood at 80% to 125% of the brand-name drug’s level. That sounds like a big window - and it is. But here’s the key: this isn’t about having 20% less drug in your body. It’s about how fast and how much of the drug gets absorbed over time. The FDA measures this using two numbers: AUC (how much drug is absorbed overall) and Cmax (how high the peak level goes).
Studies show that in practice, most generics are within 3% to 5% of the brand-name drug’s performance. That’s tiny. For most people, it makes zero difference. But for others - people taking drugs with a narrow therapeutic index - even a 5% change can be risky.
Drugs like warfarin (for blood clots), levothyroxine (for thyroid), digoxin (for heart rhythm), and phenytoin (for seizures) are in this category. Their effective dose is very close to their toxic dose. A small shift in blood levels can mean the difference between control and crisis. That’s why doctors and pharmacists often recommend sticking with the same manufacturer - brand or generic - once you’re stable.
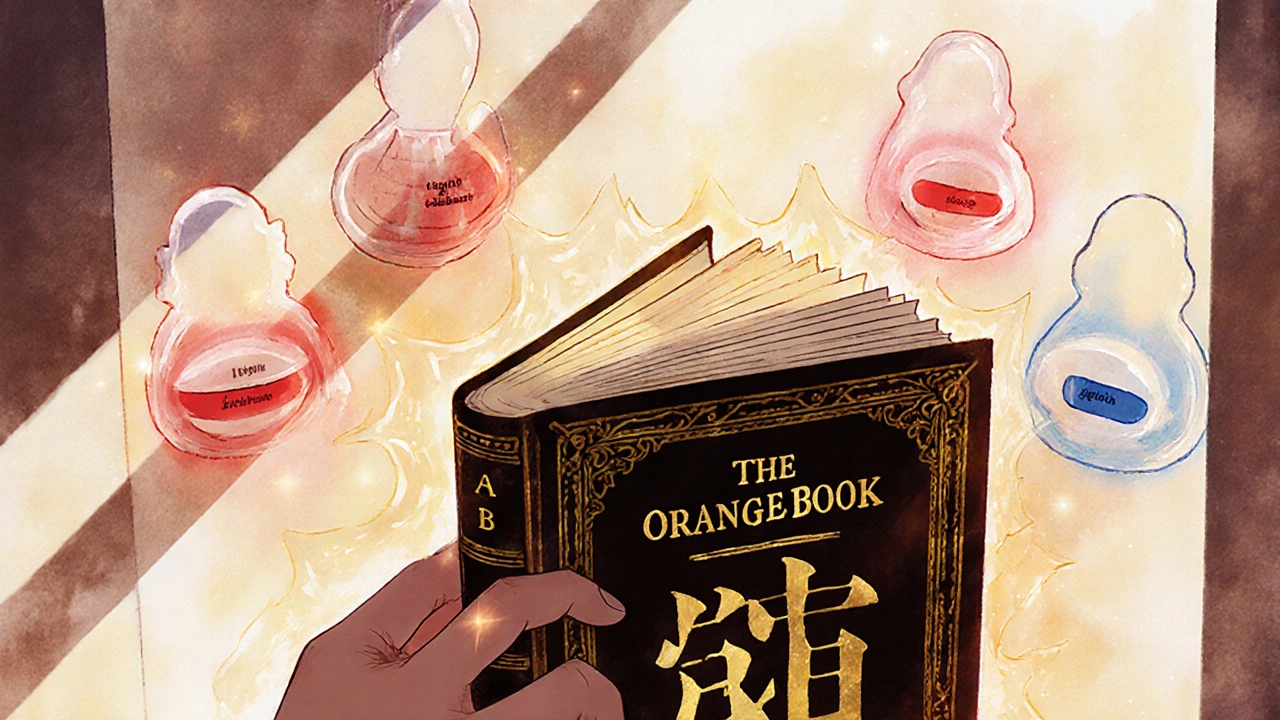
The Orange Book: Your secret tool for choosing generics
The FDA publishes a public database called the Orange Book - officially the Approved Drug Products with Therapeutic Equivalence Evaluations. It’s not a flashy website, but it’s the most important resource you’ll ever use when comparing generics.
Each generic drug is assigned a therapeutic equivalence (TE) code. Look for these two:
- AB: This means the generic has been proven bioequivalent to the brand-name drug and is considered fully interchangeable. You can switch between AB-rated generics without concern.
- B: This means the generic meets FDA standards, but there’s some uncertainty about whether it’s fully interchangeable. These are often newer generics or complex formulations. Avoid switching to a B-rated version if you’re already stable on a brand or another generic.
Pharmacists are required to check this code before substituting. But not all patients know to ask. If you’re on a high-risk medication, always ask your pharmacist: “Is this AB-rated?”
When switching generics can cause real problems
A 2017 study in Circulation: Cardiovascular Quality and Outcomes looked at patients switched from brand-name candesartan (a blood pressure drug) to different generics. In the first month after switching, adverse events increased - especially with certain generic manufacturers. Over time, the difference faded. But that first month? That’s when the body is adjusting.
Another example: levothyroxine. In 2021, the FDA issued warning letters to multiple generic manufacturers after finding inconsistent bioequivalence. The agency tightened testing requirements in March 2022. If you’re on levothyroxine and your generic was changed last year, you might have noticed changes in your energy, weight, or heart rate - even if your lab numbers were “fine.” That’s because thyroid hormone levels are extremely sensitive to small changes.
Same goes for digoxin. A 2023 report from UCSF warned that switching between generics can cause heart rhythm disturbances in some patients. The FDA has approved some generic versions as bioequivalent - but not all. And if you’ve been on the same generic for years, don’t switch unless your doctor says it’s safe.
What to do if you’re on a high-risk medication
If you take one of these drugs:
- Warfarin
- Levothyroxine
- Digoxin
- Phenytoin
- Cyclosporine
- Sirolimus
- Carbamazepine
Here’s your action plan:
- Ask your pharmacist: “Which manufacturer is this?” Write it down.
- Check the Orange Book for the TE code. If it’s AB, you’re fine. If it’s B, ask if there’s an AB option.
- Ask your doctor to write “Dispense as Written” on your prescription if you’re stable. That stops the pharmacy from switching you.
- Don’t let your medication be changed unless you’re monitored. A simple blood test (INR for warfarin, TSH for thyroid) after a switch can catch problems early.
- Stick with one manufacturer. Even if two generics are AB-rated, switching between them can cause instability. Consistency matters more than cost.
For everything else: Cost matters - and you can save big
For 90% of medications - antibiotics, statins, blood pressure pills, antidepressants - the differences between generics are negligible. The FDA’s own data shows that 80% of generic products differ from the brand by less than 5% in absorption. That’s not a problem. It’s normal.
That’s why you should always choose the lowest-cost AB-rated generic. In 2022, generics saved the U.S. healthcare system $373 billion. You’re not just saving money - you’re helping the system work better.
Here’s the trick: if your pharmacy gives you a different generic every time, ask why. Is it because they’re switching to the cheapest option? That’s fine - as long as it’s AB-rated. But if you notice side effects after a switch, speak up. Your body remembers.

What to do if your generic changes without warning
Pharmacies are allowed to substitute generics unless your doctor says “Do Not Substitute.” But in 28 U.S. states, they’re required to tell you if they’re switching to a different manufacturer. In the other 22, they don’t have to.
If you get a new bottle and the name on it looks different - even if the active ingredient is the same - don’t assume it’s the same drug. Check the pill shape, color, or imprint code. Look up the NDC (National Drug Code) on the bottle. It’s a 10-digit number. If it changed, you got a different manufacturer.
For most people, no action is needed. For those on high-risk meds, call your doctor or pharmacist immediately. Don’t wait for symptoms.
Future changes: Why labeling might soon be different
The FDA is moving toward better tracking of generic manufacturers. A proposed law called the Generic Drug Labeling Act would require each manufacturer’s version to have a unique NDC code printed clearly on the bottle. Right now, that’s not always easy to find. If this law passes, you’ll be able to tell at a glance if your generic has changed - and which one you’ve been taking.
It’s a small change, but it could prevent a lot of confusion - and maybe even save lives.
Bottom line: Know your drug, know your manufacturer
Generics aren’t “cheap knockoffs.” They’re rigorously tested, FDA-approved medicines that save billions every year. But they’re not all created equal.
For most drugs: Go for the cheapest AB-rated generic. No need to overthink it.
For high-risk drugs: Stick with one manufacturer. Don’t switch unless your doctor says so. Monitor your symptoms. Check your lab results. Ask your pharmacist for the TE code.
And always remember: your body doesn’t care about the brand name on the bottle. It cares about what’s inside - and how consistently it gets there.




sara styles
Let me tell you something the FDA doesn’t want you to know - these ‘generic’ drugs are often made in the same factories as the brand names, just repackaged under a different label. The FDA? They’re basically rubber-stamping everything because Big Pharma lobbies them into submission. I’ve seen people go from stable to seizures after a ‘switch’ - and no one gets held accountable. The NDC code? Most pharmacists don’t even know what it means. They just grab the cheapest bottle off the shelf. You think this is about health? It’s about profit margins. And you’re the lab rat.
Brendan Peterson
There’s a lot of noise here, but the core point stands: bioequivalence ranges are wide by design. The 80–125% window isn’t a loophole - it’s a statistical reality of pharmacokinetics. For most drugs, variation is negligible. But for narrow-therapeutic-index meds, consistency matters more than cost. The Orange Book is underused. I’ve seen patients on warfarin get switched three times in six months. INR spikes followed. It’s preventable. Just ask for the TE code. It’s not complicated.
Jessica M
It is imperative that patients be empowered with accurate, accessible information regarding therapeutic equivalence. The FDA’s Orange Book is an indispensable resource that remains tragically underutilized by the general public. Pharmacists are obligated to provide therapeutic equivalence codes upon request, and patients should never hesitate to inquire. For medications such as levothyroxine and digoxin, adherence to a single manufacturer is not merely advisable - it is medically essential. Consistency in formulation ensures physiological stability. One should not equate cost-efficiency with clinical safety. Your health is not a commodity.
Erika Lukacs
It’s funny how we treat medicine like it’s a vending machine - insert coin, get pill. But the body isn’t a machine. It’s a living system that remembers. Every time you switch, even if it’s ‘AB-rated,’ you’re asking your cells to relearn how to respond. We don’t question why we stick with the same therapist or the same barista who knows our order. Why do we treat our meds like disposable products? Maybe it’s not about the drug. Maybe it’s about control. And control is an illusion.
Rebekah Kryger
Okay, but let’s be real - if generics were truly interchangeable, why does the FDA even have TE codes? It’s all a scam. They want you to believe it’s about safety, but it’s really about patent loopholes. The real villain? The pharmacy benefit managers who push generics based on rebate deals, not clinical outcomes. And don’t get me started on how ‘AB’ is sometimes just a marketing term. I once got a generic that looked nothing like the last one - same NDC, different pill. Turns out, the manufacturer changed the coating. My stomach hated it. The FDA didn’t care. So yeah - ‘AB’ means nothing. Trust your body, not the label.
Victoria Short
So… just don’t switch if you’re on something like levothyroxine. Got it. Thanks for the 2,000-word essay on something I could’ve summed up in three sentences.
Eric Gregorich
I’ve been on the same generic for ten years. Same bottle. Same color. Same imprint. Then one day - different pill. Same name. Same dose. But my anxiety spiked. My heart raced. I thought I was dying. Turned out, the manufacturer changed the filler. Not the active ingredient - the filler. Cornstarch instead of lactose. I’m lactose intolerant. No one told me. No one checks. We treat pills like they’re software updates - ‘just install the new version.’ But your body isn’t a phone. It’s a temple. And someone’s replacing the incense with cheap air freshener and calling it the same thing. We’ve lost touch with the sacredness of medicine. It’s not about cost. It’s about reverence.
Koltin Hammer
There’s a quiet truth here: the system works fine for most people - and that’s why it’s allowed to be broken for the few who need it most. We optimize for the 90%, then call it progress. But the 10%? They’re the canaries. They’re the ones who feel the shift in the air before the whole mine collapses. If you’re on warfarin or levothyroxine, you’re not just taking a pill - you’re participating in a silent negotiation between chemistry and chaos. The Orange Book isn’t just a database - it’s a lifeline. And if you’re lucky enough to have access to it, don’t treat it like a footnote. Treat it like your last line of defense. Because sometimes, the difference between stability and crisis isn’t a dose - it’s a manufacturer. And no one’s coming to save you. You have to save yourself.