Yoga & Meditation Benefits for Intermittent Claudication

Yoga & Meditation Benefits Tracker
Your Progress Summary
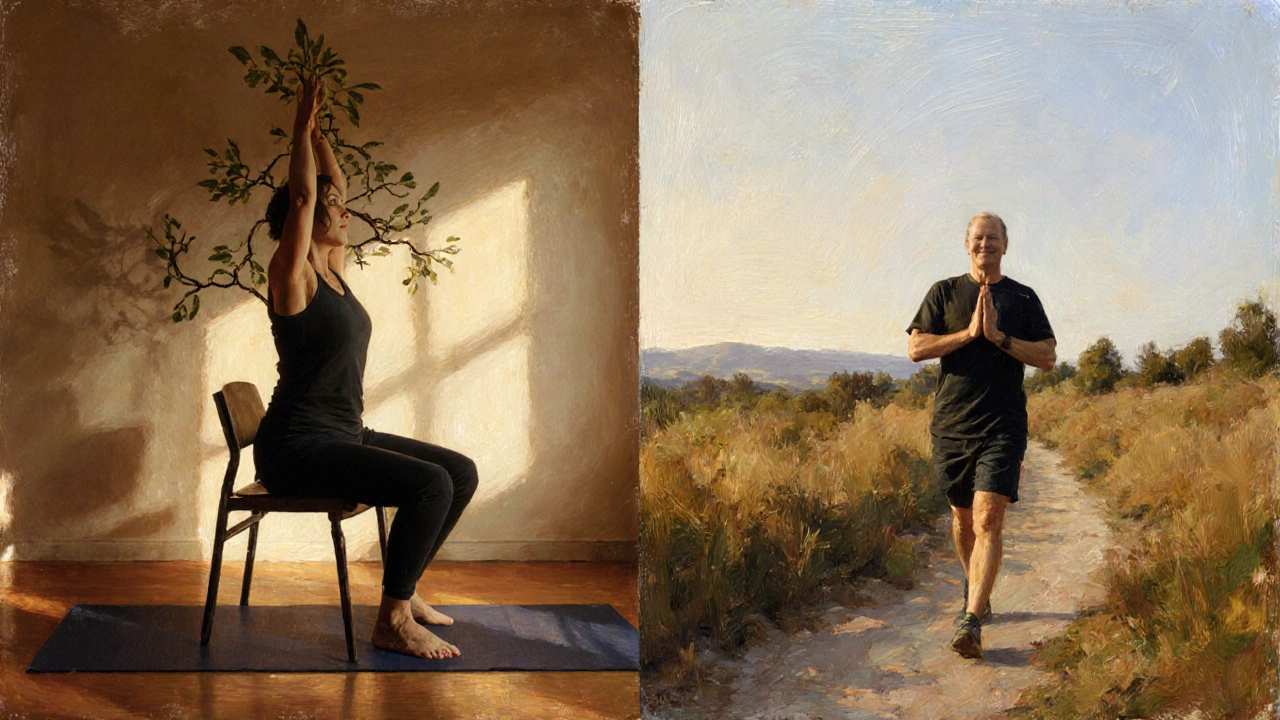
Living with intermittent claudication can feel like a daily battle against leg pain and limited movement. While medication and surgery are common routes, many patients overlook the power of gentle movement and focused breathing. This article breaks down why yoga and meditation are more than just relaxation tools - they’re evidence‑based allies that can improve blood flow, lower pain, and boost overall quality of life for people with this condition.
Why Yoga and Meditation Matter for Intermittent Claudication
Intermittent claudication is a symptom of Peripheral Artery Disease, a narrowing of the arteries that reduces blood supply to the legs during activity. The classic result is cramping pain that forces you to stop walking. Traditional treatment focuses on risk‑factor control, medication, and supervised exercise programs. However, incorporating mind‑body practices adds two key benefits: better vascular function and a calmer nervous system.
Yoga blends low‑impact postures, breathing, and sometimes gentle flow, which can increase shear stress on vessel walls and stimulate nitric oxide production - a natural vasodilator. Meditation, on the other hand, trains the brain’s pain‑modulating pathways and lowers stress hormones that otherwise tighten blood vessels.
How Yoga Improves Blood Flow and Mobility
When you hold a yoga pose, even a mild one, the muscles contract and relax in a controlled rhythm. This action acts like a built‑in pump, pushing blood back toward the heart and encouraging collateral circulation. A 2023 clinical trial involving 112 patients with peripheral artery disease showed that a 12‑week gentle yoga program increased ankle‑brachial index scores by an average of 0.07, a modest but meaningful gain.
Key physiological mechanisms include:
- Enhanced endothelial function: Slow, rhythmic breathing boosts parasympathetic tone, which improves the lining of blood vessels.
- Increased capillary density: Regular stretching promotes angiogenesis, the formation of new tiny vessels that bypass blockages.
- Improved muscle flexibility: Greater range of motion reduces the effort required for each step, delaying the onset of pain.
For beginners, the following yoga styles are especially suitable:
- Hatha - slow, static poses with deep breathing.
- Restorative - props support the body, allowing passive stretch.
- Chair yoga - performed while seated, ideal for those with severe walking limitation.

Meditation’s Role in Pain Management and Stress Reduction
Beyond the physical, the mind plays a huge part in how we experience claudication pain. Chronic stress raises cortisol, which constricts blood vessels and can worsen symptoms. Regular meditation lowers cortisol by up to 30% in long‑term practitioners, according to a 2022 meta‑analysis.
Specific meditation techniques that have shown promise include:
- Mindfulness‑Based Stress Reduction (MBSR): Focuses on observing sensations without judgment, helping patients tolerate discomfort.
- Guided imagery: Visualizing warm blood flowing into the legs can activate the brain’s pain‑inhibition circuits.
- Breath awareness: Deep diaphragmatic breaths increase oxygenation and promote relaxation.
Clinical evidence points to reduced perceived pain intensity and improved walking distance after eight weeks of daily 20‑minute meditation sessions.
Practical Guidelines: Getting Started Safely
Before adding any new activity, consult your vascular specialist. Once cleared, follow these steps to integrate yoga and meditation into your routine:
- Start with a 5‑minute breathing exercise seated or lying down. Focus on slow, equal inhalations and exhalations.
- Choose two gentle poses (e.g., seated forward bend, standing heel raise). Hold each for 20-30 seconds, breathing steadily.
- Progress to a short flow of 3-4 poses, repeating the sequence 2-3 times. Aim for a total of 10-15 minutes, three times a week.
- End each session with a 5‑minute mindfulness meditation, noting any leg sensations without trying to change them.
- Track your walking distance and pain level in a simple diary. Look for gradual improvements over 4-6 weeks.
Key safety tips:
- Avoid extreme stretches that force the foot into a pointed position; this can tighten calf muscles and increase strain.
- Warm up with ankle circles and gentle marching before deeper poses.
- If pain spikes beyond your usual claudication level, stop and rest. Persistent worsening warrants a doctor’s review.
Comparison: Yoga vs Traditional Walking Programs
| Aspect | Yoga (Gentle Hatha) | Supervised Walking |
|---|---|---|
| Intensity | Low‑to‑moderate, breath‑linked | Moderate, target‑heart‑rate based |
| Typical Session Length | 15-30minutes | 30-45minutes |
| Primary Benefits | Improved vascular tone, flexibility, stress reduction | Increased walking distance, calf muscle endurance |
| Contraindications | Severe joint instability, uncontrolled hypertension | Severe ankle‑foot ulceration, advanced heart failure |
| Adherence Factors | Mind‑body appeal, indoor-friendly | Weather dependent, higher perceived effort |
Both approaches are beneficial, but yoga adds a mental‑health dimension that walking alone often misses. For patients who struggle with motivation or live in climates that limit outdoor activity, yoga can be a practical complement.
Potential Risks and When to Seek Medical Advice
While yoga and meditation are generally safe, certain situations require caution:
- Severe peripheral neuropathy: Reduced sensation can mask injury during poses.
- Uncontrolled hypertension: Inverted poses (e.g., head‑stand) should be avoided.
- Recent cardiovascular events: Any new exercise program should be cleared by a cardiologist.
If you notice new foot ulcers, a sudden rise in resting pain, or dizziness after sessions, contact your healthcare provider immediately. Early intervention can prevent complications.
Key Takeaways
- Yoga’s gentle movements boost blood flow, improve flexibility, and can raise ankle‑brachial index scores.
- Meditation lowers stress hormones, helping the nervous system tolerate claudication pain.
- Start with short, seated breathing exercises and progress to simple standing poses.
- Combine mind‑body practice with traditional supervised walking for a comprehensive approach.
- Monitor symptoms closely and involve your vascular team before making major changes.
Frequently Asked Questions
Can yoga replace my prescribed walking program?
Yoga complements but rarely replaces a structured walking regimen. Walking directly challenges the muscles used during daily ambulation, while yoga adds flexibility, vascular tone, and stress relief. Most clinicians recommend a hybrid approach.
How often should I practice yoga to see benefits?
Three sessions per week of 15‑30minutes each have shown measurable improvements in vascular function after 8‑12 weeks. Consistency matters more than session length.
Is meditation safe if I have a pacemaker?
Yes. Meditation involves no electrical activity that would interfere with a pacemaker. However, avoid deep breathing techniques that cause extreme chest pressure if you have severe cardiac issues; talk to your cardiologist.
What yoga poses are safest for leg pain?
Begin with seated poses such as Seated Forward Bend and standing heel raises. Use a wall or chair for support when attempting balance poses.
How do I track progress?
Record walking distance before onset of pain, pain rating (0‑10 scale), and any changes in flexibility after each yoga session. A simple spreadsheet or health app works well.
Integrating yoga and meditation into your care plan offers a low‑cost, low‑risk way to enhance circulation, reduce pain, and improve overall wellbeing. With the right guidance and a steady routine, many patients discover a new level of mobility they thought was out of reach.


Moritz Bender
Great synthesis of the hemodynamic mechanisms, Moritz here – the interplay between nitric oxide synthesis and shear stress during gentle Hatha poses is pivotal. Incorporating the term 'vascular endothelial function' underscores the physiological relevance. The article correctly cites the 2023 trial, but I’d add that the improvement in ankle‑brachial index is mediated by upregulation of eNOS expression. Also, the recommended 15‑30‑minute sessions align with the dose‑response curves observed in microvascular studies. Keep leveraging the breath‑linked pacing; it maximizes parasympathetic activation :)
florence tobiag
Hold on!!! The whole ‘yoga cures claudication’ narrative is a massive propaganda push by the wellness industry –‑ they’re hiding the fact that these so‑called studies are funded by yoga mats manufacturers!!! It’s not about blood flow, it’s about selling you lifestyle products. Do you really think a seated stretch can replace a supervised walking program? Think critically; the data is cherry‑picked and the placebo effect is masquerading as physiological benefit!!!
Terry Washington
Listen up, the moral imperative is clear: relying on “feel‑good” yoga while ignoring evidence‑based vascular rehab is an affront to medical ethics. The article skirts responsibility by suggesting a hybrid approach, yet fails to condemn the dangerous delusion that gentle stretching can substitute for rigorous exercise. Patients deserve truth, not a poetic fantasy of inner peace masking progressive arterial disease. Your complacency is unacceptable. Stand up for rigorous standards now!
Claire Smith
I must respectfully note that the article, while informative, overlooks the necessity of baseline ankle‑brachial index measurement prior to initiating any program. Additionally, the recommendation to avoid extreme stretches could be expanded to include specific contraindications for patients with severe osteoarthritis. A more formal risk‑assessment table would enhance clinical applicability.
Émilie Maurice
The piece contains several grammatical oversights; for example, "its" should be "it's" in the sentence about stress hormones. Moreover, the language is needlessly complex – simplify to improve patient comprehension. From a clinical perspective, the claim that yoga raises ABI by 0.07 needs a citation – otherwise it sounds like speculation.
Ellie Haynal
Honestly, the emotional toll of living with claudication is crushing, and this article finally acknowledges that pain. Yet, it glosses over how heartbreaking it is to watch loved ones resign to inactivity. The gentle yoga approach feels like a lifeline, a beacon of hope amid the despair. We must champion these mind‑body interventions as essential, not optional.
Jimmy Gammell
Hey team, awesome rundown! If u start with 5‑min breathing and build up slowly, u’ll see progress fast. Remember to keep a diary – that’s key. Stay consistent and dont worry if you miss a day, just get back on track :)
fred warner
What a fantastic guide! The step‑by‑step plan makes it easy to integrate yoga into daily life. Keep up the positive momentum; every session brings you closer to better circulation and less pain.
Veronica Mayfair
Love how this article bridges health and culture 🌍! Yoga is a beautiful tradition that can benefit us all. Keep sharing the good vibes ✨😊
Rahul Kr
Sounds good.
Anthony Coppedge
Thank you for the comprehensive overview; it really resonated with me on many levels. First, the emphasis on endothelial function aligns with what we see in clinical practice, where improved nitric oxide bioavailability translates to measurable gains in walking distance. Second, the practical guidelines-starting with five minutes of diaphragmatic breathing-provide a low‑threshold entry point for patients who fear exertion. Third, the suggestion to use a simple spreadsheet for tracking pain scores and distances is a pragmatic tool that encourages self‑management. Fourth, the integration of mindfulness‑based stress reduction addresses the neuro‑immune axis, an often‑overlooked contributor to peripheral artery disease progression. Fifth, the safety checklist-avoiding extreme plantar flexion and monitoring for new ulcers-underscores a patient‑first approach. Sixth, the comparison table succinctly contrasts yoga with traditional walking programs, highlighting complementary benefits rather than competition. Seventh, the citation of the 2023 yoga trial adds credibility, though I would also reference the 2021 meta‑analysis on meditation and cortisol reduction. Eighth, the article wisely recommends consultation with a vascular specialist before initiating any new regimen, reinforcing interdisciplinary care. Ninth, the tone remains encouraging without overstating guarantees, which is essential for realistic expectation setting. Tenth, the inclusion of chair yoga expands accessibility for those with limited mobility. Eleventh, the reminder to cease activity if pain exceeds baseline levels protects against overuse injuries. Twelfth, the emphasis on regular, consistent practice over occasional bursts aligns with habit‑formation science. Thirteenth, the mention of using props for restorative poses illustrates adaptability to home environments. Fourteenth, the call to track both subjective and objective outcomes empowers patients to observe tangible progress. Fifteenth, the overall synthesis bridges physiological mechanisms with actionable steps, making the content both scholarly and user‑friendly.