Acyclovir Resistance: Causes, Symptoms, and Treatment Options

Ever taken an antiviral that suddenly stops working? That’s what patients and doctors face when acyclovir resistance develops. Below we unpack why it happens, how you might notice it, and what you can do when the usual pills fail.
What is acyclovir resistance?
Acyclovir resistance is a condition where the herpesvirus family no longer responds to the antiviral drug acyclovir. The drug, a nucleoside analogue, normally blocks viral DNA replication, but mutations in the virus can render the blockage ineffective. While resistance is rare in healthy adults, it becomes a real concern for immunocompromised patients, long‑term suppressive therapy users, and certain viral strains.
How does acyclovir work?
Understanding the drug helps explain why resistance emerges. Acyclovir is a synthetic analogue of guanosine. After entering infected cells, a viral enzyme called thymidine kinase (TK) adds a phosphate group, converting acyclovir into acyclovir‑monophosphate. Host enzymes then add two more phosphates, producing acyclovir‑triphosphate, which competitively inhibits viral DNA polymerase, halting DNA chain elongation.
Because the first activation step relies on viral TK, any change in that enzyme can cripple the drug’s effectiveness.
Key causes of resistance
- TK gene mutations: The most common mechanism. Deletions, point mutations, or frameshifts in the UL23 gene (which encodes TK) lead to reduced or absent enzyme activity.
- DNA polymerase mutations: Alterations in the UL30 gene can lower the binding affinity of acyclovir‑triphosphate.
- Prolonged therapy: Continuous suppressive dosing, especially in transplant recipients or HIV‑positive patients, creates selection pressure that favors resistant strains.
- Cross‑resistance: Resistance to acyclovir often predicts reduced susceptibility to related drugs like valacyclovir and famciclovir, because they share the same activation pathway.
Who is most at risk?
Not everyone who takes acyclovir will develop resistance. The highest‑risk groups include:
- HIV patients with low CD4 counts.
- Organ transplant recipients on immunosuppressants.
- Patients with hematologic malignancies undergoing chemotherapy.
- Individuals on long‑term suppressive therapy for recurrent genital herpes or herpes zoster.

Spotting the symptoms
When resistance develops, the classic signs of a herpes outbreak don’t improve despite adequate dosing. Look for:
- Lesions that persist beyond the usual 7‑10 day healing window.
- Worsening pain or new satellite lesions.
- Re‑eruption after a short symptom‑free interval while still on medication.
- Laboratory confirmation of virus in cultures despite therapy.
In immunocompromised hosts, the disease can spread internally, leading to esophagitis, pneumonitis, or encephalitis that fails to respond to standard acyclovir doses.
Confirming resistance: laboratory testing
Clinical suspicion isn’t enough; you need a lab test. Two main approaches are used:
- Phenotypic drug‑susceptibility assay: Virus isolated from a lesion is grown in cell culture and exposed to increasing concentrations of acyclovir. The lowest concentration that inhibits 50 % of viral replication (IC50) is measured. An IC50 > 10 µg/mL usually indicates resistance.
- Genotypic sequencing: PCR amplifies the TK (UL23) and DNA polymerase (UL30) genes. Sequencing then identifies known resistance‑conferring mutations such as TK‑A200V or DNA‑polymerase‑L500P.
Both methods have pros and cons. Phenotypic assays reflect actual drug response but take 5‑7 days, while genotypic testing is faster (24‑48 h) but may miss novel mutations.
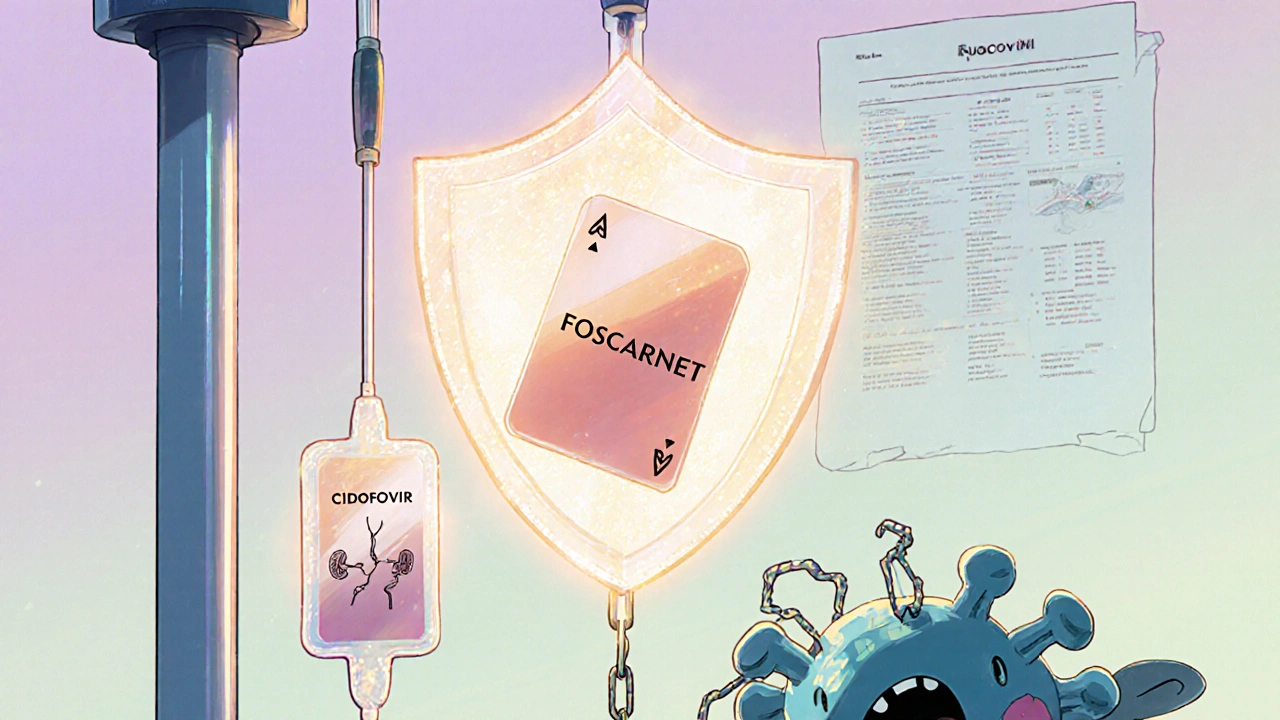
Treatment options when acyclovir fails
If testing confirms resistance, you have several alternatives. Choice depends on the virus involved, organ function, and prior drug exposure.
| Drug | Mechanism | Typical Dose | Key Advantages | Major Toxicities |
|---|---|---|---|---|
| Foscarnet | Direct DNA‑polymerase inhibitor (does not require TK activation) | 60‑90 mg/kg IV q8h | Effective against TK‑deficient strains; broad spectrum | Nephrotoxicity, electrolyte imbalance |
| Cidofovir | Nucleotide analogue; incorporated by viral DNA polymerase | 5 mg/kg IV weekly | Long‑acting; works on VZV and CMV | Severe nephrotoxicity, requires probenecid |
| Valacyclovir (high‑dose) | Prodrug of acyclovir (still TK‑dependent) | 3 g PO q8h (for severe disease) | Oral administration; better bioavailability | Limited if TK mutated; GI upset |
| Brivudine | Thymidine analogue; activated by viral TK | 125 mg PO daily | Potent against HSV‑1, less resistance reported | Potential drug‑interaction with sorivudine‑based chemotherapy |
**Foscarnet** and **cidofovir** are the go‑to IV drugs because they bypass the defective TK step. However, they demand close monitoring of kidney function and electrolytes. Oral options like high‑dose valacyclovir may still work if the resistance is partial, but they’re less reliable.
Practical management algorithm
- Confirm resistance with phenotypic or genotypic testing.
- Assess patient’s renal function and electrolyte status.
- If renal function is adequate, start foscarnet (IV) with pre‑hydration.
- For patients with poor kidney reserve, consider cidofovir with probenecid and aggressive hydration.
- Monitor serum creatinine every 48 h.
- Adjust dose if creatinine clearance < 50 mL/min.
- Re‑evaluate clinical response after 5‑7 days.
- Improvement: continue for a total of 14‑21 days.
- No improvement: reassess for mixed infection, drug levels, or alternative diagnoses.
Prevention strategies
Stopping resistance before it starts is better than fighting it later. Here are proven tactics:
- Limit suppressive therapy: Use the lowest effective dose, and consider drug holidays if the patient’s immune system is stable.
- Rotate antivirals: In transplant protocols, alternating acyclovir with ganciclovir can reduce selection pressure.
- Vaccination: The shingles vaccine (Shingrix) reduces VZV reactivation, cutting the need for antivirals.
- Early detection: Routine viral cultures in high‑risk wards enable swift identification of resistant strains.
Key take‑aways for patients and clinicians
- Resistance is rare in healthy people but common in immunocompromised hosts.
- Persistent lesions despite proper dosing should trigger resistance testing.
- Foscarnet and cidofovir are the mainstays for TK‑deficient viruses, but require kidney monitoring.
- Prevention hinges on judicious antiviral use and immunization.
Can resistant herpes infections spread to other parts of the body?
Yes. In immunocompromised patients, resistant HSV or VZV can cause esophagitis, pneumonitis, or encephalitis, all of which may not respond to standard acyclovir doses.
How long does it take to get genotypic resistance results?
Most labs can deliver PCR‑based sequencing within 24‑48 hours, allowing clinicians to adjust therapy quickly.
Is there any oral medication that works when acyclovir fails?
High‑dose valacyclovir may work if the virus retains partial TK activity, but for full resistance IV agents like foscarnet are preferred.
What monitoring is required for foscarnet therapy?
Serum creatinine, electrolytes (especially magnesium and potassium), and urine output should be checked before each dose and at least every 48 hours.
Can vaccination reduce the need for acyclovir?
The recombinant zoster vaccine (Shingrix) dramatically lowers shingles incidence, thus decreasing reliance on antivirals in older adults.


Zaria Williams
Honestly, if you’re not on a transplant list, you don’t need to worry about acyclovir resistance.
ram kumar
When you parade a wall‑of‑text about viral enzymes, you forget that most patients are just trying to get over a cold sore.
Sure, the biochemistry is fascinating, but the average person wants to know if their lesion will finally heal.
Throwing in terms like "thymidine kinase" without a simple analogy turns a helpful post into a textbook.
And let’s be real: many clinicians skim the abstract and miss the nitty‑gritty about dosing adjustments.
The article could have saved us all a lot of confusion by summarizing the key take‑aways in plain language.
Bottom line: clarity beats complexity every time.
Melanie Vargas
Great breakdown! 😊 This is exactly the kind of info that helps patients and docs stay on the same page.
Love the table – makes picking the right drug so much easier.
And the reminder about kidney monitoring? Super important. 👍
Deborah Galloway
Thanks for the thorough post! I’ve seen a few cases where the lesions just wouldn’t budge, and it was a relief to finally have a clear algorithm to follow.
If you ever need a quick handout for patients, let me know – happy to help.
Charlie Stillwell
Let’s dissect this so‑called ‘comprehensive guide’ piece by piece, because the average reader deserves clarity beyond the buzzwords.
First, you casually toss TL;DR acronyms while assuming everyone knows the intricacies of thymidine kinase, which is a delightful way to alienate the layperson.
Second, the repeated emphasis on foscarnet as the silver bullet ignores its notorious nephrotoxicity that can turn a simple outbreak into a dialysis nightmare.
Third, you gloss over the economic burden-these IV drugs cost a small fortune, and most clinics don’t have the budget to stock them for every resistant case.
Fourth, the table you included looks like a spreadsheet a CFO would draft, yet you forget to mention dosage adjustments for pediatric patients.
Fifth, the algorithm suggests pre‑hydration for foscarnet, but you omit the reality that many patients have fluid restrictions, making the recommendation impossible.
Sixth, you claim genotypic testing is faster without acknowledging the false‑negative rate that can mislead clinicians.
Seventh, the brief mention of brivudine as a ‘potent’ option fails to address its contraindication with certain chemotherapies, a potentially lethal oversight.
Eighth, your prevention tips sound like a checklist for a pharmaceutical sales pitch rather than a patient‑centered strategy.
Ninth, you overlook the psychological toll of prolonged lesions; chronic pain can lead to depression, which you barely skim over.
Tenth, you present vaccination as a ‘nice to have’ when in reality shingles vaccination can halve the incidence of VZV reactivation in the elderly.
Eleventh, you cite IC50 thresholds without explaining the clinical relevance, leaving readers to guess why 10 µg/mL matters.
Twelfth, the article never addresses the emerging data on letermovir, a newer antiviral that shows promise against resistant HSV strains.
Thirteenth, you don’t discuss monitoring protocols beyond creatinine, ignoring electrolyte shifts that can precipitate cardiac arrhythmias.
Fourteenth, the language oscillates between academic and meme‑like, making the tone jarring and untrustworthy.
Fifteenth, while you sprinkle emojis in the FAQ, you forget that the primary audience is clinicians who need sterile, data‑driven guidance.
In short, this piece is a mixed bag of useful facts buried under a mountain of omissions and editorial flair. 😤
Ken Dany Poquiz Bocanegra
Resistance isn’t just a lab curiosity – it’s a real barrier for patients on long‑term suppressive therapy.
Testing early can spare weeks of ineffective treatment.
Don’t forget to adjust doses based on renal function before jumping to foscarnet.
krishna chegireddy
Everyone acts like these antivirals are safe, but the pharma giants never tell you about the hidden side‑effects.
The real danger is the data they keep under lock, not the virus itself.
Ask yourself why we’re still using drugs discovered in the 80s.
Tamara Schäfer
I think the articel does a good job, but there are few typo's that can make it hard to read.
For example, "resistence" should be "resistance".
Also, the section on foscarnet could use a bit more detail on dosing.
Overall, very informativ and helpful.
Hope this helps other readers!
Buddy Bryan
To add a bit of nuance to Charlie’s rant, the nephrotoxicity of foscarnet can be mitigated with aggressive pre‑hydration and electrolyte replacement.
Monitoring serum creatinine every 48 hours is standard, but some centers also track magnesium and potassium daily.
When kidney function is borderline, switching to cidofovir with probenecid can be a viable alternative, though it has its own renal risks.
In practice, the choice often comes down to the patient’s overall comorbidities and the ability to tolerate IV therapy.
Hope this clarifies the trade‑offs.
Aaron Kuan
Foscarnet kills even the toughest strains
Brett Witcher
While conspiracy theories are tempting, the peer‑reviewed literature consistently shows that resistance arises from well‑characterized mutations, not hidden corporate agendas.
It is more productive to focus on evidence‑based prevention and monitoring.
Benjamin Sequeira benavente
Fantastic post! 🚀 Let’s keep the conversation going and make sure every clinician has the tools to spot resistance early.
Remember, proactive monitoring saves lives and reduces costs.
Stay motivated, stay informed!